Monday, June 6, 2011
Male Heart Disease May Be Linked to Mom's Lifetime Nutrition Risk associated, in part, with mother's body size, placenta size and shape at birth, researchers say
Male Heart Disease May Be Linked to Mom's Lifetime NutritionRisk associated, in part, with mother's body size, placenta size and shape at birth, researchers sayBy Alan Mozes THURSDAY, June 2 (HealthDay News) -- A man's heart disease risk after the age of 40 may be linked, at least in part, to his mother's body size and placenta size when he was born, a new study suggests."Chronic disease is the product of a mother's lifetime nutrition and the early growth of her child," study lead author Dr. David Barker, a professor of clinical epidemiology at the University of Southampton in the United Kingdom, said in a news release from the European Society of Cardiology. "It is not simply a consequence of poor lifestyles in later life. Rather, it is a result of variations in the normal processes of human development."The finding is reported online June 1 in the European Heart Journal by Barker, who is also a professor in cardiovascular medicine at Oregon Health and Science University, and colleagues.Indications of the maternal influence on the heart disease risk of male offspring stem from an analysis involving nearly 7,000 Finnish men who were born in Helsinki between 1934 and 1944.At that time, birth records included notations on the baby's size, the placental surface size, and other information on the mother's weight, height and age, and previous pregnancies. (The placenta -- a temporary organ that lines the uterus and feeds the baby in the womb -- is expelled at birth.)The investigators found that male heart disease risk in late adulthood appeared to rise among:Men whose mothers were short, pregnant for the first time and had relatively oval placentas (indicating that the placental development had been disrupted). Men whose mothers were tall and heavy and had relatively small placentas (which might have restricted the infants' growth mid-gestation). Men whose mothers were tall with a lower-than-normal body mass index and whose placentas were heavy relative to birth weight (the mothers' BMIs suggest that their nutrition was poor during pregnancy, Barker explained).Regardless of which combination was in play, those men with the greatest likelihood for developing heart disease as adults had tended to be relatively thin at birth. This fact, the authors suggested, was an indication that malnourishment was a factor at the time of birth."We have been able to show for the first time that a combination of the mother's body size and the shape and size of the placental surface predicts later heart disease," Barker said.Going forward, the research team intends to study abnormal development of the heart by examining pregnant women's nutritional habits and body characteristics alongside prenatal growth patterns and placenta sizes at birth.
Saturday, June 4, 2011
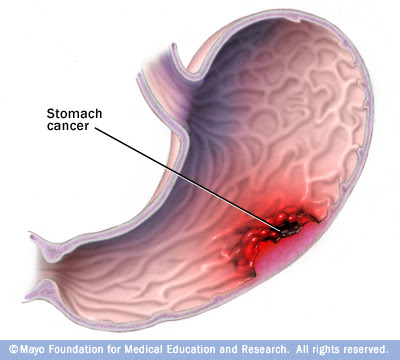
Stomach Cancer
The stomach
The stomach is a hollow organ in the upper abdomen, under the ribs.It's part of the digestive system. Food moves from the mouth through the esophagus to the stomach. In the stomach, the food becomes liquid. Muscles in the stomach wall push the liquid into the small intestine.
The wall of the stomach has five layers:
- Inner layer or lining (mucosa): Juices made by glands in the inner layer help digest food. Most stomach cancers begin in this layer.
- Submucosa: This is the support tissue for the inner layer.
- Muscle layer: Muscles in this layer contract to mix and mash the food.
- Subserosa: This is the support tissue for the outer layer.
- Outer layer (serosa): The outer layer covers the stomach. It holds the stomach in place.
Understanding cancer
Cancer begins in cells, the building blocks that make up tissues. Tissues make up the organs of the body.Normally, cells grow and divide to form new cells as the body needs them. When cells grow old, they die, and new cells take their place.
Sometimes, this process goes wrong. New cells form when the body does not need them, and old or damaged cells do not die as they should. The buildup of extra cells often forms a mass of tissue called a growth, polyp, or tumor.
Tumors in the stomach can be benign (not cancer) or malignant (cancer). Benign tumors are not as harmful as malignant tumors:
- Benign tumors:
- are rarely a threat to life
- can be removed and usually don't grow back
- don't invade the tissues around them
- don't spread to other parts of the body
- Malignant tumors:
- may be a threat to life
- often can be removed but sometimes grow back
- can invade and damage nearby organs and tissues
- can spread to other parts of the body
Stomach cancer cells can spread by breaking away from the original tumor. They enter blood vessels or lymph vessels, which branch into all the tissues of the body. The cancer cells may be found in lymph nodes near the stomach. The cancer cells may attach to other tissues and grow to form new tumors that may damage those tissues.
The spread of cancer is called metastasis. See the Staging section for information about stomach cancer that has spread.
Risk factors
When you're told that you have stomach cancer, it's natural to wonder what may have caused the disease. But no one knows the exact causes of stomach cancer. Doctors seldom know why one person develops stomach cancer and another doesn't.Doctors do know that people with certain risk factors are more likely than others to develop stomach cancer. A risk factor is something that may increase the chance of getting a disease.
Studies have found the following risk factors for stomach cancer:
- Helicobacter pylori infection: H. pylori is a bacterium that commonly infects the inner lining (the mucosa) of the stomach. Infection with H. pylori can cause stomach inflammation and peptic ulcers. It also increases the risk of stomach cancer, but only a small number of infected people develop stomach cancer.
- Long-term inflammation of the stomach: People who have conditions associated with long-term stomach inflammation (such as the blood disease pernicious anemia) are at increased risk of stomach cancer. Also, people who have had part of their stomach removed may have long-term stomach inflammation and increased risk of stomach cancer many years after their surgery.
- Smoking: Smokers are more likely than nonsmokers to develop stomach cancer. Heavy smokers are most at risk.
- Family history: Close relatives (parents, brothers, sisters, or children) of a person with a history of stomach cancer are somewhat more likely to develop the disease themselves. If many close relatives have a history of stomach cancer, the risk is even greater.
- Poor diet, lack of physical activity, or obesity:
- Studies suggest that people who eat a diet high in foods that are smoked, salted, or pickled have an increased risk for stomach cancer. On the other hand, people who eat a diet high in fresh fruits and vegetables may have a lower risk of this disease.
- A lack of physical activity may increase the risk of stomach cancer.
- Also, people who are obese may have an increased risk of cancer developing in the upper part of the stomach.
On the other hand, people who do develop the disease sometimes have no known risk factors.
symptoms of stomach cancer
Symptoms
Early stomach cancer often does not cause symptoms. As the cancer grows, the most common symptoms are:- Discomfort or pain in the stomach area
- Difficulty swallowing
- Nausea and vomiting
- Weight loss
- Feeling full or bloated after a small meal
- Vomiting blood or having blood in the stool
Diagnosis
If you have symptoms that suggest stomach cancer, your doctor will check to see whether they are due to cancer or to some other cause. Your doctor may refer you to a gastroenterologist, a doctor whose specialty is diagnosing and treating digestive problems.Your doctor will ask about your personal and family health history. You may have blood or other lab tests. You also may have:
- Physical exam: Your doctor feels your abdomen for fluid, swelling, or other changes. Your doctor also will check for swollen lymph nodes.
- Endoscopy: Your doctor uses a thin, lighted tube (endoscope) to look into your stomach. Your doctor first numbs your throat with an anesthetic spray. You also may receive medicine to help you relax. The tube is passed through your mouth and esophagus to the stomach.
- Biopsy: An endoscope has a tool for removing tissue. Your doctor uses the endoscope to remove tissue from the stomach. A pathologist checks the tissue under a microscope for cancer cells. A biopsy is the only sure way to know if cancer cells are present.
- How will the biopsy be done?
- Will it hurt?
- Are there any risks? What are the chances of infection or bleeding after the biopsy?
- When can I resume my normal diet?
- How soon will I know the results?
- If I do have cancer, who will talk to me about next steps? When?
Staging
If the biopsy shows that you have stomach cancer, your doctor needs to learn the stage (extent) of the disease to help you choose the best treatment.
Staging is a careful attempt to find out the following:
- How deeply the tumor invades the wall of the stomach
- Whether the stomach tumor has invaded nearby tissues
- Whether the cancer has spread and, if so, to what parts of the body.
- Chest x-ray: An x-ray of your chest can show whether cancer has spread to the lungs.
- CT scan: An x-ray machine linked to a computer takes a series of detailed pictures of your organs. You may receive an injection of dye. The dye makes abnormal areas easier to see. Tumors in your liver, pancreas, or elsewhere in the body can show up on a CT scan.
- Endoscopic ultrasound: Your doctor passes a thin, lighted tube (endoscope) down your throat. A probe at the end of the tube sends out sound waves that you cannot hear. The waves bounce off tissues in your stomach and other organs. A computer creates a picture from the echoes. The picture can show how deeply the cancer has invaded the wall of the stomach. Your doctor may use a needle to take tissue samples of lymph nodes.
- Laparoscopy: A surgeon makes small incisions (cuts) in your abdomen. The surgeon inserts a thin, lighted tube (laparoscope) into the abdomen. The surgeon may remove lymph nodes or take tissue samples for biopsy.
When stomach cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the primary (original) tumor. For example, if stomach cancer spreads to the liver, the cancer cells in the liver are actually stomach cancer cells. The disease is metastatic stomach cancer, not liver cancer. For that reason, it is treated as stomach cancer, not liver cancer. Doctors call the new tumor "distant" or metastatic disease.
These are the stages of stomach cancer:
- Stage 0: The tumor is found only in the inner layer of the stomach. Stage 0 is also called carcinoma in situ.
- Stage I is one of the following:
- The tumor has invaded only the submucosa. Cancer cells may be found in up to 6 lymph nodes.
- Or, the tumor has invaded the muscle layer or subserosa. Cancer cells have not spread to lymph nodes or other organs.
- Stage II is one of the following:
- The tumor has invaded only the submucosa. Cancer cells have spread to 7 to 15 lymph nodes.
- Or, the tumor has invaded the muscle layer or subserosa. Cancer cells have spread to 1 to 6 lymph nodes.
- Or, the tumor has penetrated the outer layer of the stomach. Cancer cells have not spread to lymph nodes or other organs.
- Stage III is one of the following:
- The tumor has invaded the muscle layer or subserosa. Cancer cells have spread to 7 to 15 lymph nodes.
- Or, the tumor has penetrated the outer layer. Cancer cells have spread to 1 to 15 lymph nodes.
- Or, the tumor has invaded nearby organs, such as the liver, colon, or spleen. Cancer cells have not spread to lymph nodes or to distant organs.
- Stage IV is one of the following:
- Cancer cells have spread to more than 15 lymph nodes.
- Or, the tumor has invaded nearby organs and at least 1 lymph node.
- Or, cancer cells have spread to distant organs.
What is the treatment for stomach cancer?
Treatment
The choice of treatment depends mainly on the size and location of the tumor, the stage of disease, and your general health.Treatment for stomach cancer may involve surgery, chemotherapy, or radiation therapy. You'll probably receive more than one type of treatment. For example, chemotherapy may be given before or after surgery. It's often given at the same time as radiation therapy.
You may want to talk with your doctor about taking part in a clinical trial, a research study of new treatment methods. Clinical trials are an important option for people at any stage of stomach cancer.
You may have a team of specialists to help plan your treatment. Your doctor may refer you to a specialist, or you may ask for a referral. Specialists who treat stomach cancer include gastroenterologists, surgeons, medical oncologists, and radiation oncologists. Your health care team may also include an oncology nurse and a registered dietitian.
Your health care team can describe your treatment choices, the expected results, and the possible side effects. Because cancer therapy often damages healthy cells and tissues, side effects are common. Before treatment starts, ask your health care team about possible side effects, how to prevent or reduce these effects, and how treatment may change your normal activities. You and your health care team can work together to make a treatment plan that meets your needs.
You may want to ask your doctor these questions before you begin treatment:
- What is the stage of the disease? Has the cancer spread? Do any lymph nodes show signs of cancer?
- What is the goal of treatment? What are my treatment choices? Which do you suggest for me? Why?
- What are the expected benefits of each kind of treatment?
- What can I do to prepare for treatment?
- Will I need to stay in the hospital? If so, for how long?
- What are the risks and possible side effects of each treatment? How can side effects be managed?
- What is the treatment likely to cost? Will my insurance cover it?
- How will treatment affect my normal activities? Am I likely to have eating or other problems?
- Would a research study (clinical trial) be a good choice for me?
- Can you recommend other doctors who could give me a second opinion about my treatment options?
- How often should I have checkups?
treatment for stomach cancer
Surgery
The type of surgery for stomach cancer depends mainly on where the cancer is located. The surgeon may remove the whole stomach or only the part that has the cancer.You and your surgeon can talk about the types of surgery and which may be right for you:
- Partial (subtotal) gastrectomy for tumors at the lower part of the stomach: The surgeon removes the lower part of the stomach with the cancer. The surgeon attaches the remaining part of the stomach to the intestine. Nearby lymph nodes and other tissues may also be removed.
- Total gastrectomy for tumors at the upper part of the stomach: The surgeon removes the entire stomach, nearby lymph nodes, parts of the esophagus and small intestine, and other tissues near the tumor. Rarely, the spleen also may be removed. The surgeon then connects the esophagus directly to the small intestine.
Many people who have stomach surgery feel tired or weak for a while. Your health care team will watch for signs of bleeding, infection, or other problems that may require treatment.
The surgery can also cause constipation or diarrhea. These symptoms usually can be controlled with diet changes and medicine. See the Nutrition section for information about eating after surgery.
You may want to ask your doctor these questions before having surgery:
- What kind of surgery do you recommend for me? Why?
- Will you remove lymph nodes? Will you remove other tissue? Why?
- How will I feel after surgery?
- Will I need a special diet?
- If I have pain, how will you control it?
- How long will I be in the hospital?
- Am I likely to have eating problems?
- Will I have any long-term side effects?
Chemotherapy
Most people with stomach cancer get chemotherapy. Chemotherapy uses drugs to kill cancer cells.It may be given before or after surgery. After surgery, radiation therapy may be given along with chemotherapy.
The drugs that treat stomach cancer are usually given through a vein (intravenous). You'll probably receive a combination of drugs.
You may receive chemotherapy in an outpatient part of the hospital, at the doctor's office, or at home. Some people need to stay in the hospital during treatment.
The side effects depend mainly on which drugs are given and how much. Chemotherapy kills fast-growing cancer cells, but the drugs can also harm normal cells that divide rapidly:
- Blood cells: When drugs lower the levels of healthy blood cells, you're more likely to get infections, bruise or bleed easily, and feel very weak and tired. Your health care team will check for low levels of blood cells. If your levels are low, your health care team may stop the chemotherapy for a while or reduce the dose of the drug. There are also medicines that can help your body make new blood cells.
- Cells in hair roots: Chemotherapy may cause hair loss. If you lose your hair, it will grow back after treatment, but the color and texture may be changed.
- Cells that line the digestive tract: Chemotherapy can cause a poor appetite, nausea and vomiting, diarrhea, or mouth and lip sores. Your health care team can give you medicines and suggest other ways to help with these problems. They usually go away when treatment ends.
You may want to ask your doctor these questions before having chemotherapy:
- Why do I need this treatment?
- Which drug or drugs will I have?
- How do the drugs work?
- When will treatment start?
- When will it end?
- Will I have any long-term side effects?
Radiation therapy
Radiation therapy (also called radiotherapy) uses high-energy rays to kill cancer cells. It affects cells only in the part of the body that is treated. Radiation therapy is usually given with chemotherapy to treat stomach cancer.The radiation comes from a large machine outside the body. You'll go to a hospital or clinic for treatment. Treatments are usually 5 days a week for several weeks.
Side effects depend mainly on the dose and type of radiation. External radiation therapy to the chest and abdomen may cause a sore throat, pain similar to heartburn, or pain in the stomach or the intestine. You may have nausea and diarrhea. Your health care team can give you medicines to prevent or control these problems.
It's common for the skin in the treated area to become red, dry, tender, and itchy.
You're likely to become very tired during radiation therapy, especially in the later weeks of treatment. Resting is important, but doctors usually advise patients to try to stay active, unless it leads to pain or other problems.
Although the side effects of radiation therapy can be distressing, your doctor can usually treat or control them. Also, side effects usually go away after treatment ends.
You may want to ask your doctor these questions before having radiation therapy:
- Why do I need this treatment?
- When will the treatments begin?
- When will they end?
- How will I feel during treatment?
- How will we know if the radiation treatment is working?
- Will I have any long-term side effects?
What are treatment options for cancer that blocks the digestive tract?
Cancer that blocks the digestive tract
People with advanced stomach cancer may develop a tumor that blocks the passage of food through the digestive tract. Your health care team may suggest one or more of the following options:- Stent: The doctor uses an endoscope to place a stent (a tube made of metal mesh or plastic) in your intestine. Food and liquid can pass through the center of the tube.
- Radiation therapy: Radiation therapy may help shrink the tumor that is blocking the intestine.
- Laser therapy: A laser is a concentrated beam of intense light that kills tissue with heat. The doctor uses an endoscope to place the laser in your digestive tract. The laser destroys the cancer cells blocking the digestive tract.
Cancer and its treatments may cause pain. Your health care team or a pain control specialist can suggest ways to relieve or reduce pain. Radiation therapy and pain medicine may help.
Follow-up care
You'll need regular checkups after treatment for stomach cancer. Checkups help ensure that any changes in your health are noted and treated if needed. If you have any health problems between checkups, you should contact your doctor.Your doctor will check for return of the cancer. Also, checkups help detect health problems that can result from cancer treatment.
Checkups may include a physical exam, blood tests, x-rays, CT scans, endoscopy, or other tests. If you had surgery on the stomach, your doctor may order blood tests to check the levels of certain vitamins and minerals, such as vitamin B12, calcium, and iron.
Sources of support
Learning that you have stomach cancer can change your life and the lives of those close to you. These changes can be hard to handle. It's normal for you, your family, and your friends to need help coping with the feelings that such a diagnosis can bring.Concerns about treatments and managing side effects, hospital stays, and medical bills are common. You may also worry about caring for your family, keeping your job, or continuing daily activities.
Here's where you can go for support:
- Doctors, nurses, and other members of your health care team can answer questions about treatment, working, or other activities.
- Social workers, counselors, or members of the clergy can be helpful if you want to talk about your feelings or concerns. Often, social workers can suggest resources for financial aid, transportation, home care, or emotional support.
- Support groups also can help. In these groups, people with stomach cancer or their family members meet with other patients or their families to share what they have learned about coping with the disease and the effects of treatment. Groups may offer support in person, over the telephone, or on the Internet. You may want to talk with a member of your health care team about finding a support group.
- Information specialists at 1-800-4-CANCER ( 1-800-422-6237 ) and at LiveHelp (http://www.cancer.gov/help) can help you locate programs, services, and publications. They can send you a list of organizations that offer services to people with cancer.
Stomach Cancer At A Glance
- Stomach cancer (gastric cancer) can develop in any part of the stomach and spread to other organs.
- The cause of stomach cancer is not known, but certain risk factors for stomach cancer have been identified.
- Stomach ulcers do not appear to increase a person's risk of developing stomach cancer.
- Symptoms of stomach cancer are often vague.
- Stomach cancer is diagnosed with a biopsy of stomach tissue during a procedure called an endoscopy.
- Treatment of stomach cancer depends on the size, location, and extent of the tumor, the stage of the disease, and the health of the patient.
Lead Poisoning Symptoms
According to the Centers for Disease Control and Prevention, lead poisoning affects 250,000 children under 5 years of age in the United States. Furthermore, there is no evidence that the rates of exposure of children to lead is decreasing. Lead gradually accumulates in the body due to long-term exposure in the environment. It is especially dangerous to newborns, infants, and small children because the effects on the developing brain may be permanent and irreversible. Initial symptoms in infants and children include:
The risk of lead exposure all depends upon where you live. Lead paint was often used in houses built before the early 1970s, when lead paint was made illegal. Some older water pipes were connected with lead solder that could leach into the drinking water. Antique toys and those made outside the United States also may contain lead.
Screening for lead poisoning begins with routine visits to a health care professional. The American Academy of Pediatrics developed a three question test to find kids at risk for lead poisoning:
The CDC also has lead screening policies. In 2000, they recommended that all children younger than 5 years of age receiving Medicaid assistance be screened for lead poisoning. That has been adjusted in the last year to ask state and local governments and health agencies to assess high risk communities and decide which individuals are best to screen for possible lead poisoning. The common thread is that many people living in older low income housing units and their children have increased risk for lead exposure.
It isn't just the house that can make a difference; it can be the neighborhood as well. Factories that use lead to make batteries and other industrial components can use lead in the manufacturing process and can contaminate the air and ground. While this is better regulated in Western countries, recent events in China should be a reminder why zoning and environmental laws exist. In 2009, a smelting plant in Hunan located less than a mile from a school was found to be the source of over 2,000 children sickened with lead poisoning. In May 2011, a battery plant was found to be the source of lead poisoning in Hangzhou.
Adults are not immune from lead poisoning. Again living in an older house is a prime risk factor. Work exposure may be a concern. Lead solder is used in making stained glass windows and older paint on antique furniture can release lead when refurbishing occurs.
Symptoms in adults are similar to those in children and include:
A quarter million kids have been found to have toxic levels of lead in their bodies. The goal is to identify those who are unaware that they have been poisoned. It's up to parents, health care professionals, caregivers, and public health officials to find these children, treat them, and minimize future risk.
- irritability,
- abdominal pain,
- vomiting, and
- constipation.
The risk of lead exposure all depends upon where you live. Lead paint was often used in houses built before the early 1970s, when lead paint was made illegal. Some older water pipes were connected with lead solder that could leach into the drinking water. Antique toys and those made outside the United States also may contain lead.
Screening for lead poisoning begins with routine visits to a health care professional. The American Academy of Pediatrics developed a three question test to find kids at risk for lead poisoning:
- Does your child live in or regularly visit a house or child care facility built before 1950?
- Does your child live in or regularly visit a house or child care facility built before 1978 that is being or has recently been renovated or remodeled (within the last 6 months)?
- Does your child have a sibling or playmate who has or did have lead poisoning?
The CDC also has lead screening policies. In 2000, they recommended that all children younger than 5 years of age receiving Medicaid assistance be screened for lead poisoning. That has been adjusted in the last year to ask state and local governments and health agencies to assess high risk communities and decide which individuals are best to screen for possible lead poisoning. The common thread is that many people living in older low income housing units and their children have increased risk for lead exposure.
It isn't just the house that can make a difference; it can be the neighborhood as well. Factories that use lead to make batteries and other industrial components can use lead in the manufacturing process and can contaminate the air and ground. While this is better regulated in Western countries, recent events in China should be a reminder why zoning and environmental laws exist. In 2009, a smelting plant in Hunan located less than a mile from a school was found to be the source of over 2,000 children sickened with lead poisoning. In May 2011, a battery plant was found to be the source of lead poisoning in Hangzhou.
Adults are not immune from lead poisoning. Again living in an older house is a prime risk factor. Work exposure may be a concern. Lead solder is used in making stained glass windows and older paint on antique furniture can release lead when refurbishing occurs.
Symptoms in adults are similar to those in children and include:
- headache,
- nausea,
- memory loss,
- muscle weakness, and
- tingling in the arms and legs.
A quarter million kids have been found to have toxic levels of lead in their bodies. The goal is to identify those who are unaware that they have been poisoned. It's up to parents, health care professionals, caregivers, and public health officials to find these children, treat them, and minimize future risk.
Ferritin Blood Test
Ferritin Blood Test Facts
- The ferritin test measures the level of ferritin, the major iron storage protein in the body.
- The ferritin test is a simple blood test.
- High levels of ferritin can indicate an iron storage disorder, such as hemochromatosis, or a chronic disease process.
- Low levels of ferritin are indicative of iron deficiency, which causes anemia (a reduction in the number of red blood cells).
What is ferritin?
Ferritin is a body protein that is used to store iron. It is the major iron storage protein of the body, so measurement of ferritin levels is an indirect way to measure the amount of iron stored by the body. Ferritin has the shape of a hollow sphere that permits the entry of a variable amount of iron for storage (as ferric hydroxide phosphate complexes).What is the ferritin blood test?
The ferritin test uses venous blood that is withdrawn as for any routine blood test. No special preparation for the test is necessary.The test is sometimes ordered together with other tests to help evaluate the body's iron stores, such as an iron level or a total iron binding capacity test.
What are normal results for a ferritin test?
The results may vary slightly among laboratories, but in general, normal ferritin levels are 12-300 nanograms per milliliter of blood (ng/mL) for males and 12-150 ng/mL for females.What does an elevated ferritin level mean?
High levels of ferritin can be indicative of an iron storage disorder such as hemochromatosis.Hereditary hemochromatosis is an inherited (genetic) disorder in which there is excessive accumulation of iron in the body (iron overload). This condition affects approximately one in 240 to 300 Caucasians in the Unites States. In individuals with hereditary hemochromatosis, the daily absorption of iron from the intestines is greater than the amount needed to replace losses. Since the normal body cannot increase iron excretion, the absorbed iron accumulates in the body.
- A man with hemochromatosis can accumulate 20 grams of total body iron by age 40 to 50 (the normal iron content for the body is 3-4 grams). The excess iron deposits in the joints, liver, testicles, and heart, which causes damage to these organs, and causes signs and symptoms of hemochromatosis.
- Women with hemochromatosis accumulate iron at a slower rate than men because they lose more iron than men due to iron loss from menstruation. Therefore, they typically develop signs and symptoms of organ damage due to excess iron 10 years later then men.
- sexual dysfunction,
- heart failure,
- joint pains,
- liver cirrhosis,
- diabetes mellitus,
- fatigue, and
- darkening of skin.
Other causes of a high ferritin level are chronic inflammatory conditions such as liver disease or rheumatoid arthritis, or some types of cancer.
What does a low ferritin level mean?
Low levels of ferritin are seen in iron deficiency. Without enough iron, the body cannot produce sufficient levels of hemoglobin, a component of red blood cells that allows them to carry oxygen. Iron deficiency anemia is the result. Mild anemia may not produce symptoms at all. More serious cases of anemia can produce symptoms such as:- shortness of breath,
- fatigue,
- dizziness,
- pale skin, and
- fast heartbeat
HPV Test (Cervista Human Papillomavirus Infection Test in Women)
Cervista HPV Test Facts
- A subgroup of the human papillomaviruses (HPVs) are known to cause cancers of the uterine cervix and other genital areas, the so-called "high risk" HPVs.
- The Cervista test is used to diagnose the presence of DNA from the "high-risk" HPVs in cervical samples.
- The sample for the test is taken in the same way that a Pap smear test is performed.
- There are two Cervista tests available, Cervista HPV 16/18, which identified the two HPV types most likely to cause cancer, and Cervista HPV HR, which identifies all "high-risk" HPV types.
- Cervista testing is not recommended for routine screening; rather, it is used in combination with physical examination, medical history, and other testing to help make decisions about management and follow-up on a case-by-case basis.
What is human papillomavirus (HPV)?
Of the more than 100 types of papillomaviruses (HPVs) that infect humans, more than 40 types can infect the anogenital tract (genital tract and anus) of men and women and cause genital warts (known as condylomata acuminata or venereal warts). A subgroup of the HPVs that infect the anogenital tract (genital tract and anus) can lead to precancerous changes in the uterine cervix and cause cervical cancer or other genital cancers in women. The HPV types that cause cervical cancer also have been linked with both anal and penile cancer in men.The most common HPV types that infect the anogenital tract are HPV types 6, 11, 16, and 18 (HPV-6, HPV-11, HPV-16, and HPV-18), although other HPV types can also infect the anogenital tract. Among these, HPV-6 and HPV-11 are most commonly associated with benign lesions such as genital warts and mild dysplasia of the cervix (potentially precancerous changes in the appearance of cervical cells under a microscope) and are termed "low-risk" HPV types. In contrast, HPV-16 and HPV-18 are the types found in the majority of cervical and anogenital cancers as well as severe dysplasia of the cervix. These belong to the so-called "high-risk" group of HPVs. Twelve other HPV types have also been identified as causes of cervical and other genital cancers, although these are less common that HPV-16 and -18.
HPV infections are transmitted primarily by sexual intimacy, and the risk of infection increases as the number of sexual partners increase.
What is the Cervista HPV test?
The Cervista HPV test, manufactured by Hologic, is a test that is used to identify the presence of human papillomavirus (HPV) genetic material, or DNA, in cervical samples, such as samples taken during Pap screening or colposcopy. The Cervista test was approved by the U.S. Food and Drug Administration in March of 2009 and was the first DNA test approved by the FDA for detection of HPV in women.Two different tests are available, known as Cervista HPV 16/18 and Cervista HPV HR. Cervista HPV 16/18 is used to diagnose the presence of DNA from the two most common HPV types associated with cancer, HPV 16 and 18, while Cervista HPV HR is used to diagnose all 14 "high risk" or cancer-associated HPV types. The choice for which test to use depends on what information the patient's physician wants to collect.
How is the HPV test done?
For the Cervista test, a sample is taken from the cervix in the same way that a sample for Pap testing is obtained. It can be performed at the same time as Pap testing or colposcopy. There is no special preparation needed for the test, although women should try to schedule Cervista and other screening tests about two weeks after their last menstrual period and try to avoid having the test performed during the menstrual period. Results are typically ready in about the same time as normal Pap screening results.Who should be tested for HPV?
The Cervista test is not used for routine screening of all women and is not intended to be a stand-alone test. It is not recommended for testing in women under 30 years of age who have normal cytology (Pap) results. Cervista is designed for use in women age 30 and older or women with unclear or borderline Pap screening results, such as ASC-US (atypical squamous cells of unknown significance) or low grade squamous intraepithelial lesions (LSIL). It can provide more information about the risk of cervical cancer for women who may have precancerous changes of the cervix.According to the manufacturer, the Cervista test "should be used in conjunction with clinical information derived from other diagnostic and screening tests, physical examinations, and full medical history in accordance with appropriate patient management procedures."
How are the results of an HPV test interpreted?
A positive test result does not mean that a woman will definitely get cervical cancer.The results of the test are used to help estimate a woman's risk of developing cervical cancer or to estimate the severity or risk of findings that may not be clear from physical examination and Pap screening. As discussed previously, the results of the Cervista HPV test are not interpreted alone but in combination with Pap testing, medical history, and physical examination. The test gives one more piece of information to help the health care practitioner make the best decisions about further monitoring and management for each woman on a case-by-case basis.
Irritable Bowel Syndrome (IBS) Triggers and Prevention
Irritable bowel syndrome (IBS) triggers and prevention introduction
By taking steps to prevent the symptoms of irritable bowel syndrome (IBS), it is possible to lead a productive, healthy life. With some planning, you can avoid IBS triggers that cause symptom flares. Your doctor can provide a complete treatment plan for IBS prevention.Print out this list of common IBS triggers and prevention strategies. Keep it handy for reference. It may help you identify your personal triggers in your IBS symptom journal. Triggers and symptoms may vary depending on your type of IBS. And when you're having a bad day, remember to persist with healthy management of your condition.
"Realize that it's not always smooth sailing. That's a part of IBS," says Leslie Bonci, MPH, RD, author of the American Dietetic Association Guide to Better Digestion. "You can't beat yourself up."
1. Diet Triggers for IBS Constipation
Some foods can worsen IBS-related constipation. These include:- Refined breads and cereals
- Refined foods such as chips and cookies
- Drinks such as coffee, carbonated drinks, and alcohol
- High-protein diets - Learn about the healthy foods on a high protein diet.
- Gradually boost fiber intake by two to three grams per day until you're eating 20 to 35 grams per day. Good sources of fiber include whole grain bread and cereals, beans, fruits, and vegetables.
- Consume a moderate amount of foods higher in sorbitol, such as dried plums and prune juice.
- Drink eight 8-ounce glasses of plain water a day.
- Try ground flaxseed. It can be sprinkled on salads and cooked vegetables.
2. Diet Triggers for IBS Diarrhea
Some foods can worsen IBS-related diarrhea. These include:- Too much fiber, especially insoluble fiber found in the skin of fruits and vegetables
- Food and drinks with chocolate, alcohol, caffeine, fructose, or the sugar substitute sorbitol
- Carbonated drinks
- Large meals
- Fried and fatty foods
- Food and drinks with dairy
- Foods with wheat -- Some people may be allergic or have a negative reaction to gluten
- Eat a moderate amount of soluble fiber. It adds bulk to the colon and can help prevent spasms. Good sources are whole wheat breads, oats, barley, brown rice, pasta, the flesh of fruit (as opposed to the skin), and dried fruits.
- Don't consume foods with extreme temperatures, such as ice-cold water and steaming hot soup, in the same meal.
- Stay away from broccoli, onions, and cabbage. They can cause gas, which can make diarrhea sufferers feel worse.
- Eat smaller portions.
- Drink six to eight glasses of plain water a day, but drink the water an hour before or after meals, not with meals.
- Consult with your doctor or a dietitian if you suspect you may have a wheat allergy.
3. Stress and Anxiety Triggers for IBS
Stress and anxiety can exacerbate IBS symptoms such as constipation, diarrhea, stomach pain, and bloating. Different things cause stress for different people. Stress can include:- Problems at work
- Commutes
- Problems at home
- Financial problems
- A sense that things are beyond your control
- Practice healthy living. Eat a well-balanced diet that is appropriate for your IBS. Get regular exercise and enough sleep.
- Do something fun. Listen to music, read, shop, or take a walk.
- Try behavioral therapy. Learn how to calm yourself down with the help of techniques such as relaxation therapy, biofeedback, hypnotherapy, cognitive behavioral therapy, and psychotherapy.
- Talk to people. If you feel comfortable doing so, tell your family members, close friends, boss, and co-workers about your IBS. They may provide vital support. Plus, the conversation may prevent any misunderstandings when your symptoms flare up and you are not able to meet expectations.
- Plan ahead. Ease worries about going out lest your symptoms flare up. Get up earlier if you know IBS makes you late for work. If you are driving, map your route so that you know locations of bathrooms. At social events, choose aisle seats close to the facilities. Know what's on the menu so you can eat beforehand if the food will not be agreeable to you.
4. Drugs That Can Trigger IBS
Some drugs can trigger spasms of the colon and symptoms of IBS. These spasms can lead to constipation or diarrhea.- Antibiotics, especially after prolonged use
- Antidepressants
- Medicine containing sorbitol, such as cough syrup
- Talk with your doctor about switching to a drug that won't worsen your IBS symptoms. Don't stop taking a drug without consulting with your doctor.
- If an antidepressant is worsening your diarrhea or constipation, talk with your doctor about switching medicine. Older antidepressants (called tricyclic antidepressants) can cause constipation. One type of newer antidepressant (called selective serotonin reuptake inhibitors, which include Prozac and Zoloft) can cause diarrhea. Your doctor can help you find an antidepressant that will not worsen your IBS symptoms.
5. Menstrual Triggers for IBS
Studies show that women with IBS tend to have worse symptoms during their periods. There's not a lot of information about preventing this type of trigger, but doctors may recommend certain strategies to ease pain and discomfort during your period.Prevention Strategies:
- Oral contraceptives. Some brand names are Ortho Tri-Cyclen, Lo/Ovral, and Alesse. These drugs can regularize periods. Side effects may include upset stomach, vomiting, stomach cramps or bloating, diarrhea, and constipation. Work with your doctor to find a pill that works for you without causing side effects.
- Premenstrual dysphoric disorder (PMDD) drugs. These include drugs also used to treat depression, such as Sarafem, Paxil CR, and Zoloft. PMDD is a severe form of PMS. These drugs adjust levels of serotonin, a brain chemical thought to be out of balance during certain phases of a woman's cycle.
Pregnancy Planning
Pregnancy Planning Facts
- Pregnancy planning can address issues of nutrition, vitamins, body weight, exercise, and potentially harmful medications and illnesses as well as immunizations and genetic counseling.
- Women who take folic acid at least four weeks prior to conception can reduce their baby's risk of birth defects of the spinal cord and skull by 70%.
- Alcohol has been implicated in infertility, early miscarriage, and birth defects.
- Certain acne medications and other prescription and OTC medications can cause birth defects.
- Babies of older women have an increased risk of having chromosomal abnormalities.
- The timing of sexual intercourse in relation to ovulation does not influence the gender of the baby.
What is pregnancy planning and why is it important?
Having a baby is one of the most important events in a woman's life. Women considering pregnancy are encouraged to start planning for the pregnancy with their doctors early. This early planning process is called pregnancy planning. The goals of pregnancy planning are to create a healthy environment for the fetus and to prevent birth defects and other pregnancy related problems to the greatest extent possible. The issues addressed during pregnancy planning include nutrition, vitamins, body weight, exercise, avoidance of certain medications and alcohol, immunizations, and genetic counseling. Even though many women will have normal pregnancies without any planning, pregnancy planning improves the chances of a smooth pregnancy and a healthy baby. Unfortunately, many more women who are anticipating conceiving do not seek prior medical consultation.Pregnancy planning can help prevent exposure of the mother to potentially harmful medications or substances during the early days of pregnancy. The baby's organs begin developing as early as 17 days after conception, and the fertilized egg begins to grow even before the first day of the missed period. Some women continue to have light bleeding that may be mistaken for a menstrual period during the first few months of pregnancy and may not even realize that they are pregnant. Others may not recognize that they are pregnant until they experience weight gain or abdominal enlargement. By then, they may have already been exposed to medications or substances potentially harmful to the fetus.
In addition to avoiding medications and substances that are potentially harmful to the fetus, other important health issues are addressed during pre-pregnancy planning.
- Conditions such as diabetes, high blood pressure, kidney disease, thyroid disease, and heart disease in the mother are controlled to optimize pregnancy outcome.
- The status of the woman's immunity against German measles (rubella) and varicella (chickenpox) is also determined. Women lacking rubella antibodies are immunized before conceiving (see medical issues below). Women who are not immune to varicella (chickenpox) can be vaccinated, but should wait 30 days after vaccination before becoming pregnant.
- Women who are carriers of the hepatitis B virus can be identified by blood tests, and their infants can be protected from hepatitis B infection by immunizations at the time of delivery. Women with HIV (human immunodeficiency virus) infection should take certain medications during pregnancy to decrease not only their risks but those of the fetus as well.
What are pregnancy symptoms?
There are both symptoms and signs of pregnancy. These symptoms and signs depend upon the time in pregnancy. In the first trimester of pregnancy, the first sign of pregnancy is most often a missed menstrual period. If a sexually active woman's periods are generally regular, missing a period for a week or more is presumptive evidence of pregnancy.Early symptoms of pregnancy also include feelings of breast swelling and tenderness, and nausea sometimes with vomiting. "Morning sickness" does not always occur in the morning, and the nausea of pregnancy can occur at any time of day. Many women become fatigued early in pregnancy, and some may feel abdominal enlargement (bloating).
Early in pregnancy, the woman may feel she has to urinate frequently, especially at nighttime, and she may leak urine when coughing, sneezing or laughing. This is also normal later in pregnancy and is not a problem.
Other changes characteristic of pregnancy include the deepening color of the areola (area surrounding the nipple), increased body temperature, the so-called "mask of pregnancy" (darkening of skin on the forehead, bridge of the nose, or cheekbones), and a dark line going down from the middle of the central abdomen area to the pubic area. Eventually, enlargement of the abdomen is a normal feature of the growing fetus.
What is a pregnancy calculator and calendar?
A pregnancy calendar or calculator can allow a pregnant woman to understand what is happening to her body and to the developing embryo or fetus at each stage of pregnancy. Most pregnancy calendars explain the changes of pregnancy on a week-to-week level and can be found online or in print form. In many cases, pregnancy calendars contain photos or diagrams to illustrate the appearance of the fetus at each stage.How effective are home pregnancy tests?
At-home pregnancy tests, first introduced in 1975, are very accurate and reliable when used correctly. These tests measure the presence of the hormone human chorionic gonadotropin in the urine, which, when present, is indicative of pregnancy. The same hormone is measured in blood and urine pregnancy tests available at clinics and doctors' offices. Currently, the blood test is the most specific and sensitive pregnancy test available, although urine tests have become increasingly sensitive. For example, home urine tests may be able to detect the pregnancy hormone at 8 to 9 days after conception, or a few days before the missed menstrual period.While many manufacturers claim that their home pregnancy tests are 99% accurate, a number of factors influence the accuracy of these kits. Studies have shown that false negative results may occur when very low levels of the pregnancy hormone are present, and that home test kits from different manufacturers differ in their sensitivity for detection of the very low levels of the pregnancy hormone in the early days of pregnancy. If a woman takes a home pregnancy test too soon, the result may be negative even though she is in the first stages of pregnancy. A repeat test should always be performed a week later if a home test is negative and a woman suspects that she might be pregnant.
How can diet and nutrition affect early pregnancy?
The developing fetus receives its nutrition from the mother's blood. Therefore high fat diets and some vegetarian diets are discouraged during pregnancy because they may not provide all the nutrition needed for the developing fetus. Bulimia, anorexia nervosa and other eating disorders in the mother are addressed and treated. Weight reduction diets are avoided during pregnancy. Excess intake of sugar, alcohol, megavitamins, and caffeine are also avoided Because a "safe" amount of caffeine has never been confirmed to date, it is best to avoid caffeine entirely. Women who feel strongly that they need some coffee are advised to drink no more than one cup per day. There is no proof that 1 to 2 cups of coffee daily cause pregnancy complications.Listeria is a type of bacteria found in contaminated food that can cause miscarriage and other problems in a fetus. Because of the danger of getting a listeria infection, pregnant women should avoid unpasteurized milk, soft cheeses, cold cuts, and undercooked or raw animal foods. In addition, fruits and vegetables should be washed completely prior to consumption.
Phenylketonuria is an inherited disease that affects the utilization of a certain protein component in foods. This disorder can be detected by a blood test. Mothers with phenylketonuria may give birth to developmentally disabled children unless their diets are strictly controlled to exclude phenylalanine.
Megavitamins contain double or even triple the recommended daily allowances of vitamins and minerals. High doses of vitamin A have been implicated in producing birth defects. The better idea is to avoid megavitamins and instead follow the recommendation that has proven benefit: take a prenatal vitamin containing folic acid.
Folic acid intake in the mother prior to, and during pregnancy has been shown to reduce the risk of birth defects involving the brain and spinal cord. The United States Public Health Service recommends folic acid for all women of child-bearing capacity. Studies have shown that if folic acid is begun at least 4 weeks prior to conception, the risk of birth defects of the spinal cord and skull can be reduced by more than 70%. In women with or even without a history of having infants with birth defects of the spinal cord or skull, folic acid should be taken one month before conception and continued through the 12th week of pregnancy. In fact, continuing prenatal vitamins through pregnancy and even through nursing is probably wise. These prenatal vitamins are available over-the-counter. If a particular brand makes you feel nauseated, simply switch to another brand or try taking the vitamin at night.
Because of the risks of mercury poisoning and nervous system damage in the fetus from contaminated fish, pregnant women are advised to eliminate consumption of certain types of fish that are known to be high in mercury, including shark, swordfish, tilefish, and king mackerel. Tuna steaks, made from large tuna, may also have high mercury levels. Canned tuna is made from smaller fish that typically have lower levels of mercury than larger fish.
Pregnancy Planning
How does alcohol affect pregnancy?
Alcohol has been implicated in infertility, early miscarriage, as well as in birth defects. The amount of alcohol consumption necessary to cause these problems is not known, and varies among women. Some women can drink excessively and have normal infants. Others consume considerably less alcohol but still give birth to babies with cognitive disabilities and/or other birth defects. It is generally believed that the greater the amount of alcohol consumed during pregnancy, the greater the risk of pregnancy-related problems and birth defects.It is recommended that pregnant women avoid all consumption of alcohol. Fetal alcohol spectrum disorders are a group of conditions reflecting the possible effects of prenatal exposure to alcohol. The FASDs include fetal alcohol syndrome (FAS), alcohol-related birth defects (ARBD), and alcohol-related neurodevelopmental disabilities (ARND). Fetal alcohol syndrome (FAS) is the extreme end of the fetal alcohol spectrum disorders and is a leading cause of cognitive disabilities.
How do high blood pressure and diabetes affect pregnancy?
Elevated blood pressure (hypertension) that is present before pregnancy can interfere with growth of the fetus and increase the risk of fetal death. Therefore, controlling blood pressure with carefully chosen blood pressure medications is important during pregnancy and before conception.In addition, underlying hypertension can increase the risk for a condition called preeclampsia, a potentially very dangerous complication of pregnancy. It is sometimes difficult for doctors to distinguish between high blood pressure alone and high blood pressure occurring from preeclampsia. For those reasons, and given the risk of birth defects from many of the blood pressure medications, women with high blood pressure who become pregnant should be followed very carefully by a medical expert who is familiar with this type of situation. Ideally, medication would be switched to a relatively safe medication before the woman even becomes pregnant.
Poorly controlled diabetes can lead to high blood sugar levels. High blood sugar levels during early pregnancy can lead to miscarriages and birth defects. Therefore, controlling diabetes is important for a good pregnancy outcome, and the blood sugar should ideally be controlled before becoming pregnant. It is important to consider that control of blood sugar during pregnancy is important, but control prior to pregnancy may be just as important.
Oral diabetes medications may be dangerous to the fetus, but insulin is not dangerous to the fetus. Insulin is the key treatment for diabetes during pregnancy. Not only is insulin safe to the baby and mother, but it also helps prevent the complications that the baby could have suffered from the mother's sugar being uncontrolled. Insulin is usually substituted for pills as soon as a woman with diabetes is considering pregnancy. The ideal time to control blood sugar is before pregnancy, because control of sugar levels even in early pregnancy (when the mother does not yet know she is pregnant) is important for the developing baby's health.
What are examples of commonly-used medications that are dangerous in pregnancy?
Many women do not know that over-the-counter medications can be dangerous. In fact, many prescription and over-the-counter medications harm the fetus very early in pregnancy at a time that the mother does not even know she is pregnant. Even aspirin use by the mother can cause defects in the fetus. For this reason, as soon as pregnancy is being contemplated, women should avoid all over-the-counter and prescription medications until reviewed with their doctor.Acne medications, such as isotretinoin (Accutane) can cause birth defects, and should be discontinued before conception. Since many medications and substances can affect fetal growth and development, pregnancy planning is important so that potentially harmful substances can be stopped before conceiving.
Unplanned pregnancy during oral contraceptive use is not felt to pose a significant danger to the fetus, although deliberate use of oral contraceptives during pregnancy is not advisable. Women who become pregnant during oral contraceptive use have the same risk of birth defects in their newborns as the general population of women, in the range of 2% to 3%.
How do kidney and heart disease affect pregnancy?
Because pregnancy is associated with an increase in blood volume and an increase in cardiac output as well as other changes in the circulatory system, many types of heart disease may worsen or be associated with poor outcome during pregnancy. While many mild chronic heart conditions may be well tolerated during pregnancy, other conditions pose a significant risk to mother and fetus. Women with preexisting heart disease should always consult an expert when planning a pregnancy to examine their own degree of risk, potential outcomes, and treatment options.What infections affect pregnancy?
Certain infections during early pregnancy can cause birth defects in the fetus. Rubella (German measles) virus infection during early pregnancy can cause birth defects and even miscarriages. Therefore, women of child bearing age are tested for blood antibodies against this virus. Women lacking rubella virus antibodies are susceptible to rubella infection, and should be vaccinated against this virus. Pregnancy should be avoided for one month after vaccination, due to the theoretical concern that the vaccine virus itself may cause fetal damage.Toxoplasmosis is a small parasite that is transmitted through cat feces and raw meats, especially pork. Toxoplasmosis, like the rubella virus, can cause severe birth defects if the infection occurs during early pregnancy. Women planning pregnancy should avoid raw meat and avoid handling the cat litter box. Many people have been exposed to toxoplasmosis without even knowing it. As a result, they develop a protective immunity from the "silent" infection. Women who have a blood test that is positive for toxoplasmosis immunity can be reassured that they will not develop toxoplasmosis complications during pregnancy.
Hepatitis B is the only type of hepatitis that is known to affect the newborn infant.
Female healthcare workers, dental assistants, and others exposed to hepatitis B should receive hepatitis B vaccination to avoid chronic infection by this virus. The majority of hepatitis B virus infections resolve spontaneously without treatment. Patients whose disease resolves completely are no longer contagious. Approximately 10% of hepatitis B virus infections do not resolve, and become chronic. Patients chronically infected with hepatitis B virus may have no symptoms of liver disease early on, but they remain contagious. Over time, chronic hepatitis B infection can lead to liver cirrhosis and/or liver cancer.
Women with chronic hepatitis B infection can transmit the virus to their babies at birth. Babies infected are at risk of developing chronic liver disease, liver cirrhosis, and liver cancer in later life. Currently, infants born to mothers infected with the hepatitis B virus are given both the hepatitis B antibodies and hepatitis B vaccinations at birth for protection. Therefore, pregnant women are often tested for signs of hepatitis B infection, even if they do not have any symptoms or knowledge of past infection. The babies of infected mothers detected in this manner would receive special care at (and after) delivery.
Cytomegalovirus (CMV) is a common viral infection worldwide that often does not produce any symptoms. Women who become infected or have a reactivation of a previous infection during pregnancy may pass the infection along to their babies. Congenital CMV infection is the most common congenital viral infection. Although the majority of infected infants will not have any symptoms, up to 20% will have symptoms that may include an enlarged spleen, jaundice, or rash. Rarely, involvement of many organs may occur resulting in severe illness or disability.
Genital herpes may also result in the passage of the infection to the infant at the time of delivery. The risk of transmission is increased if the genital lesions are from a herpesvirus (HSV) infection acquired during the pregnancy, rather than simply a reactivation of previous disease. HSV infection can have multiple effects in the newborn. Disease may be limited to the eyes, skin and mouth; may be localized to the central nervous system; or may be widespread and involve many organs. Treatment involves administration of antiviral medications to the newborn and supportive care.
Parvovirus B19 is a virus that causes the condition known as Fifth disease, a common mild disease of childhood. Transmission is by droplets in the air (respiratory secretions) or through blood. Pregnant women who have not previously had fifth disease should avoid contact with those who have it because parvovirus B-19 can infect a fetus prior to birth. Although no birth defects have been reported as a result of fifth disease, it can cause the death of an unborn fetus. This occurs in less than 5% of pregnant women who become infected with the virus.
When traveling to a foreign country, it is important to determine what diseases are common, whether vaccines are needed, and whether they are safe during pregnancy. Human immunodeficiency virus (HIV) infection can be passed from a mother to her baby. The chances of this happening are decreased substantially with certain medication programs during pregnancy. Pregnant women are routinely offered testing for HIV infection. Women with previously undetected infection who are found to have HIV infection can be given special medication to try to protect the baby. At the same time, the medication may benefit the health of the mother herself.
Varicella, or chickenpox, can cause pneumonia or even death in older adults and in pregnant women. Varicella vaccine is available for women who are not immune to chickenpox. Women who had chickenpox in the past do not need a vaccine because they are immune. Women who are not sure if they are immune can receive a blood test to determine immunity status. A vaccine would be given if the blood test showed they were not immune.
Is it safe to exercise during pregnancy?
Recommendations from the American College of Obstetrics and Gynecology say that pregnant women who have an uncomplicated pregnancy should participate in at least 30 minutes of moderate exercise on most, if not all, days of the week. A few exceptions are noted: ice hockey, kickboxing, soccer, and horseback riding probably should be avoided because they are activities with higher risk of trauma to the abdomen. Also, scuba diving poses a risk of decompression sickness ("the bends") to the fetus and should be avoided. Exercise programs should be discussed with the monitoring health care professional.Elevated temperatures can have adverse effects on the development of the fetus. Therefore, hot tubs and sauna baths should be avoided when trying to conceive and during pregnancy.
Angina
Introduction to angina
Chest pain is a common symptom that is caused by many different conditions. Some causes require prompt medical attention, such as angina, heart attack, or tearing of the aorta. Other causes of chest pain that may not require immediate medical intervention include spasm of the esophagus, gallbladder attack, or inflammation of the chest wall. An accurate diagnosis is important in providing proper treatment to patients with chest pain.The diagnosis and treatment of angina is discussed below, as well as the diagnosis of other causes of chest pain that can mimic angina.
What is angina, and what are the symptoms of angina?
Angina (angina pectoris - Latin for squeezing of the chest) is chest discomfort that occurs when there is a decreased blood oxygen supply to an area of the heart muscle. In most cases, the lack of blood supply is due to a narrowing of the coronary arteries as a result of arteriosclerosis.Angina is usually felt as:
- pressure,
- heaviness,
- tightening,
- squeezing, or
- aching across the chest, particularly behind the breastbone.
Patients may also suffer:
- indigestion,
- heartburn,
- weakness,
- sweating,
- nausea,
- cramping, and
- shortness of breath.
Angina is classified in one of two types: 1) stable angina or 2) unstable angina.
Stable angina
Stable angina is the most common type of angina, and what most people mean when they refer to angina. People with stable angina have angina symptoms on a regular basis and the symptoms are somewhat predictable (for example, walking up a flight of steps causes chest pain). For most patients, symptoms occur during exertion and commonly last less than five minutes. They are relieved by rest or medication, such as nitroglycerin under the tongue.
Unstable angina
Unstable angina is less common and more serious. The symptoms are more severe and less predictable than the pattern of stable angina. Moreover, the pains are more frequent, last longer, occur at rest, and are not relieved by nitroglycerin under the tongue (or the patient needs to use more nitroglycerin than usual). Unstable angina is not the same as a heart attack, but it warrants an immediate visit to your healthcare provider or hospital emergency department as further cardiac testing is urgently needed. Unstable angina is often a precursor to a heart attack.
What causes angina?
The most common cause of angina is coronary artery disease. A less common cause of angina is spasm of the coronary arteries.Coronary artery disease
Coronary arteries supply oxygenated blood to the heart muscle. Coronary artery disease develops as cholesterol is deposited in the artery wall, causing the formation of a hard, thick substance called cholesterol plaque. The accumulation of cholesterol plaque over time causes narrowing of the coronary arteries, a process called arteriosclerosis. Arteriosclerosis can be accelerated by smoking, high blood pressure, elevated cholesterol, and diabetes. When coronary arteries become narrowed by more than 50% to 70%, they can no longer meet the increased blood oxygen demand by the heart muscle during exercise or stress. Lack of oxygen to the heart muscle causes chest pain (angina).
Coronary artery spasm
The walls of the arteries are surrounded by muscle fibers. Rapid contraction of these muscle fibers causes a sudden narrowing (spasm) of the arteries. A spasm of the coronary arteries reduces blood to the heart muscle and causes angina. Angina as a result of a coronary artery spasm is called "variant" angina or Prinzmetal angina. Prinzmetal angina typically occurs at rest, usually in the early morning hours. Spasms can occur in normal coronary arteries as well as in those narrowed by arteriosclerosis.
Coronary artery spasm can also be caused by use/abuse of cocaine. The spasm of the artery wall caused by cocaine can be so significant that it can actually cause a heart attack.
What are other causes of chest pain?
In caring for patients with chest pain, the doctor distinguishes whether the pain is related to a lack of oxygen to the heart muscle (as in angina or heart attack), or is due to another process. Many conditions are considered that can cause chest pain which is similar to that of a heart attack or angina. Examples include the following:- Pleuritis (pleurisy): Inflammation of the lining of the lungs (pleuritis) causes sharp chest pain, which is aggravated by deep breathing and coughing. Patients often notice shortness of breath, in part due to their shallow breathing to minimize chest pain. Viral infections are the most common causes of pleurisy. Other systemic inflammatory conditions, such as systemic lupus, can also cause pleurisy.
- Pericarditis: Pericarditis is inflammation of the lining around the heart. Symptoms of pericarditis are similar to that of pleuritis.
- Pneumonia: Pneumonia (bacterial infection of the lung) causes fever and chest pain. Chest pain in bacterial pneumonia is due to an irritation or infection of the lining of the lung (pleura).
- Pulmonary embolism: blood clots travel from the veins of the pelvis or the lower extremities to the lung, the condition is called pulmonary embolism. Pulmonary embolism can cause death of lung tissue (pulmonary infarction). Pulmonary infarction can lead to irritation of the pleura, causing chest pain similar to pleurisy. Some common causes of blood clots in these veins is deep vein thrombosis (prolonged immobility, recent surgery, trauma to the legs, or pelvic infection).
- Pneumothorax: Small sacs in the lung tissue (alveoli) can spontaneously burst, causing pneumothorax. Symptoms of pneumothorax include sudden, severe, sharp chest pain and shortness of breath. One common cause of pneumothorax is severe emphysema.
- Mitral valve prolapse: Mitral valve prolapse is a common heart valve abnormality, affecting 5% to 10% of the population. MVP is especially common among women between 20 to 40 years of age. Chest pain with MVP is usually sharp but not severe. Unlike angina, chest pain with MVP rarely occurs during or after exercise, and usually will not respond to nitroglycerin.
- Aortic dissection: The aorta is the major vessel delivering blood from the left ventricle to the rest of the body. Aortic dissection (tearing of the aorta wall) is a life-threatening emergency. Aortic dissection causes severe, unrelenting chest and back pain. Young adults with aortic dissection usually have Marfan's syndrome, an inherited disease in which an abnormal form of the structural protein called collagen causes weakness of the aortic wall. Older patients develop aortic dissection typically as a result of chronic, high blood pressure, in addition to generalized hardening of the arteries (arteriosclerosis).
- Costochondritis, rib fractures, muscle strain or spasm: Pain originating from the chest wall may be due to muscle strain or spasm, costochondritis, or rib fractures. Chest wall pain is usually sharp and constant. It is usually worsened by movement, coughing, deep breathing, and direct pressure on the area. Muscle spasm and strain can result from vigorous, unusual twisting and bending. The joints between the ribs and cartilage next to the breastbone can become inflamed, a condition called costochondritis. Fractured ribs resulting from trauma or cancer involvement can cause significant chest pain.
- Nerve compression: Compression of the nerve roots by bone spurs as they exit the spinal cord can cause pain. Nerve compression can also cause weakness and numbness in the upper arm and chest.
- Shingles (herpes zoster infection of the nerves): Shingles is nerve irritation from the infection, which can cause chest pain days before any typical rash appears.
- Esophageal spasm and reflux: The esophagus is the long muscular tube connecting the mouth to the stomach. Reflux, or regurgitation of stomach contents and acid into the esophagus can cause heartburn and chest pain. Spasm of the muscle of the esophagus can also cause chest pain which can be indistinguishable from chest pain caused by angina or a heart attack. The cause of esophageal muscle spasm is not known. Pain of esophageal spasm can respond to nitroglycerin in a similar manner as angina.
- Gallbladder attack (gallstones): Gallstones can block the gallbladder or bile ducts and cause severe pain of the upper abdomen, back and chest. Gallbladder attacks can mimic the pain of angina and heart attack.
- Anxiety and panic attacks: Anxiety, depression, and panic attacks are frequently associated with chest pain lasting from minutes to days. The pain can be sharp or dull. It is usually accompanied by shortness of breath, or the inability to take a deep breath. Emotional stress can aggravate chest pain, but the pain is generally not related to exertion, and is not relieved by nitroglycerin. These patients often breath too fast (hyperventilate), causing lightheadedness, numbness, and tingling in the lips and fingers. Coronary artery disease risk factors are typically absent in these patients. Since there is no test for panic attacks, patients with chest pain usually undergo tests to exclude coronary artery disease and other causes of chest pain.
Angina
Why is it important to establish the diagnosis of angina?
Angina is usually a warning sign of the presence of significant coronary artery disease. Patients with angina are at risk of developing a heart attack (myocardial infarction). A heart attack is the death of heart muscle precipitated by the complete blockage of a diseased coronary artery by a blood clot.During angina, the lack of oxygen (ischemia) to the heart muscle is temporary and reversible. The lack of oxygen to the heart muscle resolves and the chest pain disappears when the patient rests. In contrast, the muscle damage in a heart attack is permanent. The dead muscle turns into scar tissue when healed. A scarred heart cannot pump blood as efficiently as a normal heart, and can lead to heart failure.
Up to 25% of patients with significant coronary artery disease have no symptoms at all, even though they clearly lack adequate blood and oxygen supply to the heart muscle. These patients have "silent" angina. They have the same risk of heart attack as those with symptoms of angina.
How is angina diagnosed?
The electrocardiogram (EKG, ECG) is a recording of the electrical activity of the heart muscle, and can detect heart muscle which is in need of oxygen. The EKG is useful in showing changes caused by inadequate oxygenation of the heart muscle or a heart attack.Exercise stress test
In patients with a normal resting EKG, exercise treadmill or bicycle testing can be useful screening tools for coronary artery disease. During an exercise stress test (also referred to as stress test, exercise electrocardiogram, graded exercise treadmill test, or stress ECG), EKG recordings of the heart are performed continuously as the patient walks on a treadmill or pedals on a stationary bike at increasing levels of difficulty. The occurrence of chest pain during exercise can be correlated with changes on the EKG, which demonstrates the lack of oxygen to the heart muscle. When the patient rests, the angina and the changes on the EKG which indicate lack of oxygen to the heart can both disappear. The accuracy of exercise stress tests in the diagnosis of significant coronary artery disease is 60% to 70%. If the exercise stress test does not show signs of coronary artery disease, a nuclear agent (thallium) can be given intravenously during exercise stress test. The addition of thallium allows nuclear imaging of blood flow to different regions of the heart, using an external camera. A reduced blood flow in an area of the heart during exercise, with normal blood flow to the area at rest, signifies significant artery narrowing in that region of the heart.
Stress echocardiography
Stress echocardiography combines echocardiography (ultrasound imaging of the heart muscle) with exercise stress testing. Like the exercise thallium test, stress echocardiography is more accurate than an exercise stress test in detecting coronary artery disease. When a coronary artery is significantly narrowed, the heart muscle supplied by this artery does not contract as well as the rest of the heart muscle during exercise. Abnormalities in muscle contraction can be detected by echocardiography. Stress echocardiography and thallium stress tests are both about 80% to 85% accurate in detecting significant coronary artery disease.
When a patient cannot undergo exercise stress test because of neurological or orthopedic difficulties, medications can be injected intravenously to simulate the stress on the heart normally brought on by exercise. Heart imaging can be performed with a nuclear camera or echocardiography.
Cardiac catheterization
Cardiac catheterization with angiography (coronary arteriography) is a technique that allows x-ray pictures to be taken of the coronary arteries. It is the most accurate test to detect coronary artery narrowing. Small hollow plastic tubes (catheters) are advanced under x-ray guidance to the openings of the coronary arteries. Iodine contrast "dye" is injected into the arteries while an x-ray video is recorded. Coronary arteriography gives the doctor a picture of the location and severity of coronary artery disease. This information can be important in helping doctors select treatment options.
CT coronary angiogram
CT coronary angiography is procedure that uses an intravenous dye that contains iodine, and CT scanning to image the coronary arteries. While the use of catheters is not necessary (thus the term "noninvasive" test applies to this procedure), there are still some risks involved, including the following:
- Patients allergic to iodine
- Patients with abnormal kidney function
- Radiation exposure which is similar to, if not greater than, that received with a conventional coronary angiogram.
- at high risk for developing coronary disease (cigarette smokers, those with genetic risk, high cholesterol levels, hypertension, or diabetes),
- who have unclear results with exercise stress tests or other testing, or
- who have symptoms suspicious of coronary disease
What are the treatment options for angina patients?
Treatment options include:- rest,
- medications (nitroglycerin, beta blockers, calcium channel blockers),
- percutaneous transluminal coronary angioplasty (PTCA), or
- coronary artery bypass graft surgery (CABG).
Angina medications
Nitroglycerin
Resting, nitroglycerin tablets (placed under the tongue), and nitroglycerin sprays all relieve angina by reducing the heart muscle's demand for oxygen. Nitroglycerin also relieves spasm of the coronary arteries and can redistribute coronary artery blood flow to areas that need it most. Short-acting nitroglycerin can be repeated at five minute intervals. When 3 doses of nitroglycerin fail to relieve the angina, further medical attention is recommended. Short-acting nitroglycerin can also be used prior to exertion to prevent angina.Longer-acting nitroglycerin preparations, such as Isordil tablets, Nitro-Dur transdermal systems (patch form), and Nitrol ointment are useful in preventing and reducing the frequency and intensity of episodes in patients with chronic angina. The use of nitroglycerin preparations may cause headaches and lightheadedness due to an excess lowering of blood pressure.
Beta Blockers
Beta blockers relieve angina by inhibiting the effect of adrenaline on the heart. Inhibiting adrenaline decreases the heart rate, lowers the blood pressure, and reduces the pumping force of the heart muscle, all of which reduce the heart muscle's demand for oxygen. Examples of beta blockers include:- acebutolol (Sectral)
- atenolol (Tenormin)
- bisoprolol (Zebeta)
- metoprolol (Lopressor, Lopressor LA, Toprol XL)
- nadolol (Corgard)
- propranolol (Inderal)
- timolol (Blocadren)
- worsening of asthma,
- excess lowering of the heart rate and blood pressure,
- depression,
- fatigue,
- impotence,
- increased cholesterol levels, and
- shortness of breath due to diminished heart muscle function (congestive heart failure).
Calcium Channel Blockers
Calcium channel blockers relieve angina by lowering blood pressure, and reducing the pumping force of the heart muscle, thereby reducing muscle oxygen demand. Calcium channel blockers also relieve coronary artery spasm. Examples of calcium channel blockers include:- amlodipine (Norvasc)
- bepridil (Vascor)
- diltiazem (Cardizem)
- felodipine (Plendil)
- isradipine (Dynacirc)
- nicardipine, (Cardene)
- nifedipine (Adalat, Procardia)
- nimodipine (Nimotop)
- nisoldipine (Sular)
- verapamil (Calan)
- swelling of the legs,
- excess lowering of the heart rate and blood pressure, and
- depressing heart muscle function.
Other anti-anginal drugs
Ranolazine (Ranexa) is indicated for the treatment of chronic angina. Ranexa may be used with beta-blockers, nitrates, calcium channel blockers, antiplatelet therapy, lipid-lowering therapy, ACE inhibitors, and angiotensin receptor blockers.
Subscribe to:
Posts (Atom)